An Operation Rescue Exposé by Cheryl Sullenger
St. Louis, MO — In their legal effort to stay open in the wake of the Missouri Department of Senior Services’ decision not to renew their abortion facility license, Reproductive Health Services Planned Parenthood filed a set of documents with the Missouri Administrative Hearing Commission that included a declaration (marked as Exhibit B) by abortionist Colleen McNicholas, who now serves as full time Medical Director for Planned Parenthood of the St. Louis Region and Southwest Missouri as of July 1, 2019. In that declaration, McNicholas attempts to refute deficiencies cited by the DHSS related to four women that suffered botched or failed abortions at RHS Planned Parenthood in St. Louis.
Given McNicholas’ pattern of deceptive behavior and willingness to risk the health and safety of patients, as detailed in Part One of this report, her declaration must be viewed with skepticism.
Operation Rescue reviewed the declaration and found several points that raised red flags as to McNicholas’ veracity.
McNicholas makes dubious excuses for several deficiencies noted in the 62-page Statement of Deficiencies dated May 28, 2019, and gives a defense for RHS Planned Parenthood’s participation in failed or botched abortions for Patients 1, 2, 3, and 12.
Required pelvic exams
Missouri requires that a pelvic exam be done at the health assessment appointment 72 hours prior to abortions where women also receive informed consent and ultrasound exams.
McNicholas insisted in her declaration that the state demanded RHS Planned Parenthood to conduct two pelvic exams on women. Media statements were made by McNicholas and other RHS Planned Parenthood staff stating that Missouri was forcing them to “sexually assault” women seeking abortions.
This was inaccurate and purposely meant to foment outrage and hysteria.
“We either have to ask patients to subject themselves to a state sanctioned, essentially, sexual assault or they can’t have an abortion here in Missouri,” McNicholas stated publicly.
If McNicholas was committing “sexual assault” against her patients by conducting two pelvic exams before abortions, it was not because she was required to by law, but because she chose to in order to make a political point.
Here is the actual text of 19 CSR 30-30.050 regarding pelvic exams as it existed when the Statement of Deficiencies was issued on June 13, 2019, that requires only one pelvic exam prior to abortions, not the two wrongly claimed by McNicholas:
(D) A written medical history shall be obtained for each patient. A health assessment including a pelvic examination shall be performed. Pregnancy shall be confirmed by clinical evidence and laboratory tests. This information shall be used in determining the duration of gestation, identifying preexisting medical or other complications, and detecting any factors which could influence the choice of the procedure, anesthesia, or preoperative and postoperative management. If the physician determines gestation is beyond the first trimester, an ultrasound examination shall be performed and results shall be recorded in the patient’s medical record.
DHSS Director Randall Williams, in an effort to be a reasonable person, issued an emergency order on June 21, 2019, modifying the rule to allow for the pelvic exam to be conducted at either the 72 hour health assessment appointment, or just prior to the abortion as RHS Planned Parenthood claimed was its policy.
Patient 1
An ultrasound exam found Patient 1 to be 7 weeks 4 days into her pregnancy during a health assessment appointment at RHS Planned Parenthood on August 29, 2019.
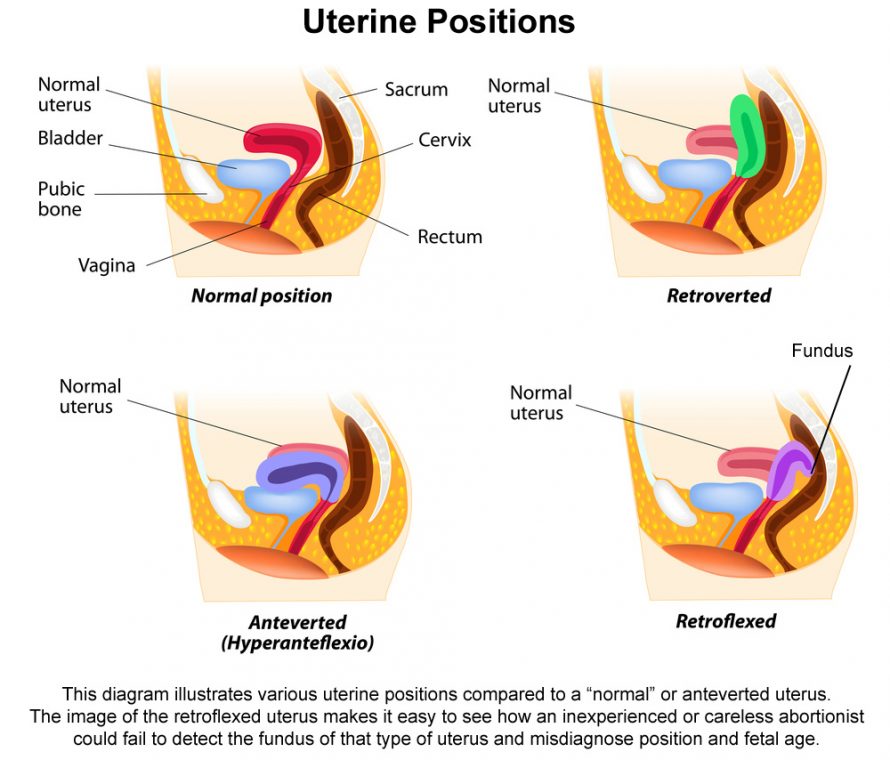
On September 5, 2019, she returned for a surgical abortion. By then Patient 1’s baby was 8 weeks, 5 days gestation, or 61 days. A pelvic exam conducted by Staff F, a physician resident, noted in the medical records that the uterine orientation was anteverted (facing forward) with the size of “less than 6 weeks,” which was obviously incorrect according to RHS Planned Parenthood’s own ultrasound results.
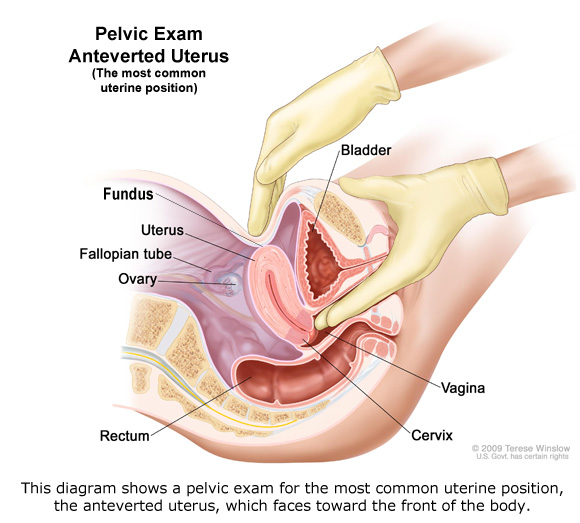
The woman’s uterus was later determined to be anteverted and severely retroflexed (lower part bent forward with the upper body of uterus bent toward the woman’s back). The pre-born baby was located near the top part of the uterus in the area behind the bend in the uterus.
It was obvious that Staff F never manually detect the fundus (very top) of the uterus during her failed pelvic exam of Patient 1, leading to the misdiagnosis.
Nevertheless, Patient 1 was subjected to a surgical abortion that was “completed with difficulty,” with no tissue returned according to the medical records cited in the deficiency report.
The somewhat unusual anatomy accounted for the failure of the first surgical procedure, which was done under the erroneous impression that the uterus was tilted forward, as most women’s uteri are.
The DHSS cited RHS Planned Parenthood for the failed pelvic exam that should have detected the correct orientation of the uterus and the larger pregnancy.
The faulty determination that the size of the uterus was consistent with a pregnancy under six weeks should have raised red flags before the first abortion was ever attempted.
However, McNicholas defended the resident’s faulty pelvic exam and diagnosis.
“DHSS’s contention that an inaccurate pelvic exam contributed to the change of treatment plan for Patient #1 is also false. In fact, documentation throughout the chart by both the fellow and attending physicians were consistent in documenting the pelvic exam. There is simply no basis to conclude the pelvic exam was not accurately performed.” [Except for the incorrect determination of uterine size and orientation!]
“As we explained in the POC, DHSS’s suggestion to the contrary reflects a lack of understanding of medicine and basic female anatomy,” McNicholas stated in her declaration. “The resident physician did not find the patient had an anteflexed uterus, as DHSS suggests; she correctly documented anteversion in the patient’s record, which is not inconsistent with my finding of retroflexion.”
However, the terms “anteflexed” or “anteflexion” do not appear in the Statement of Deficiencies.
McNicholas’ statement that the pelvic exam produced accurate results is, of course, ridiculous. But so are her further excuses about the failed medication abortion on this same patient.
Failed abortions
McNicholas defied reality when she insisted that the first surgical abortion did not fail. In order to make a statement like that, she had to redefine “failed abortion.”
“In the case of a surgical abortion, a failed abortion is understood to occur after the procedure has been completed and the patient has left the facility believing the procedure was successful, when in fact the patient remains pregnant,” stated McNicholas.
This contrived definition allows her to gaslight the court into questioning whether the first unsuccessful attempt to abort Patient 1’s pre-born baby was actually a “failed” attempt. Meanwhile, back in the world of reality, the first attempted abortion was indeed a failed abortion because it failed to kill the baby, which was the entire purpose of the abortion in the first place.
Deceptive use of complication rates
After the first attempt at a surgical abortion failed, Patient 1 was given abortion-inducing drugs and sent home. On September 7, 2019, she returned to RHS Planned Parenthood complaining that the abortion drugs did not work. At that time, McNicholas conducted a third abortion (second surgical), which was successful.
McNicholas admits that there were five known cases of failed abortions 2,500 surgical abortions done at RHS Planned Parenthood in 2019, not counting the failed abortion on Patient 1. She further stated that medication abortions fail in 0.7 percent of cases, citing information from the U.S. Food and Drug Administration, indicating that failed abortions are among the rarest of complications.
However, that is not entirely true.
A study conducted with the National Institutes of Health on women aborting at Planned Parenthood facilities explained that very low failure rate applied only to women under 60 days pregnant who took the abortion drugs buccally, which means that the pills were placed between the cheek and gums and allowed to dissolve.
Effectiveness of the buccal misoprostol-mifepristone regimen was 98.3% for women with gestational ages below 60 days. The oral misoprostol-mifepristone regimen, used by 278 women with a gestational age below 50 days, had a success rate of 96.8%.
Planned Parenthood facilities usually administer the drugs orally, which diminishes the efficacy rate.
Patient 1 was 61 days pregnant, so her risks of having a failed abortion with oral administration of abortion-inducing drugs were much greater than even the 3.2 percent failure rate for women eleven days earlier in their pregnancies.
Lack of Supervision
When McNicholas was interviewed by the DHSS investigator, she was asked if she was present during Staff F’s pelvic exam, to which McNicholas responded, “I don’t know.”
This led the DHSS question whether abortion trainees were being properly supervised.
McNicholas essentially admits as much. Her declaration contained the following statement in one of the document’s footnotes.
“In all cases, I am always present on the surgical floor either in the procedure room or nearby, depending on the patient’s needs and the trainee physician’s skill,” she said.
“Imagine allowing a surgical trainee to conduct an operation while the trainer is in another room. That is exactly the situation that McNicholas describes occurring at RHS Planned Parenthood as a matter of course,” said Operation Rescue President Troy Newman. “No wonder we have documented over 70 medical emergencies there.”
Patient 2
Patient 2 went to Planned Parenthood on May 21, 2018, and received informed consent for a surgical abortion signed by Staff B. An ultrasound indicated she was 9 weeks and 4 days pregnant. She returned to the abortion facility on May 26, 2018, and received a surgical abortion at 10 weeks gestation from Staff B without ultrasound assistance.
The medical record for Patient 2 indicated that the abortion was completed without difficulty and that the ultrasound indicated the patient’s baby was 10 weeks and 2 days gestation. It further noted that “some” fetal parts were seen by Staff B.

Patient 2 contacted RHS Planned Parenthood three weeks later to report that she believed she was still pregnant. A second abortion attempt was scheduled two weeks later – a five-week delay from the first failed abortion. By then, Patient 2’s growing baby, whose heartbeat was detected, was now 15 weeks and 2 days.
McNicholas justified the first botched gross examination of fetal remains this way:
As we explained in our POC, and as I stated in my interview, gross tissue exams are imperfect and even highly trained physicians and pathologists are not always able to accurately confirm a completed abortion from a gross tissue exam, particularly at earlier gestations.
Staff B conducted the second surgical abortion and this time certified that “all” fetal parts were observed, indicating the second abortion was complete.
McNicholas insists that Patient 2 had been pregnant with twins and that the first abortion only removed one of the babies.
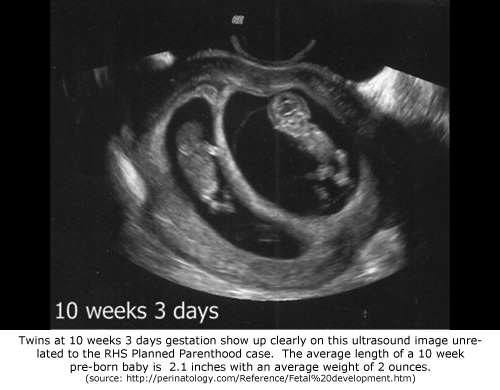
However, no twin was ever detected during the initial ultrasound exam, which should have clearly showed two babies, if twins were present. Nor was the possibility of twins detected by pelvic examination, which should have discovered a uterus larger than normal for a woman carrying twins in their eleventh week of gestation.
Two pathology reports were prepared from the two abortions.
The pathologist admitted he did not compare the second report with the first one to determine why this woman had another abortion five weeks after the first one. There was also no communication between the pathologist and RHS Planned Parenthood about the unusual double abortion.
The DHSS contends that the first pathology examination was incorrect. During an investigation, the pathology lab was cited for failing to conduct competency tests on those conducting pathology exams, who also lacked adequate training.
Two days after her second abortion attempt, Patient 2 was admitted to the hospital after seeking help at the emergency room. She has become septic due to complications to the second abortion. Sepsis is a serious infection that spreads to the whole body through the bloodstream and can have an adverse effect on vital tissues and organs.
McNicholas’ explanation of a twin pregnancy was considered insufficient due to the lack of diagnostic evidence a twin pregnancy ever existed.
It is possible that the incorrect pathology report and abortionists notes that fetal parts were seen after the first abortion were simply the product of lazy record-keeping where results that were expected were recorded.
Patient 3
Patient 3 reported to RHS Planned Parenthood for her initial informed consent appointment on July 19, 2018. Staff E, Colleen McNicholas, signed her consent form and performed a pelvic exam that indicated her baby was 6 to 8 weeks gestation. An ultrasound found her to be 6 weeks pregnant.
On July 25, 2018, Staff A – the same resident trainee responsible two of Patient 1’s failed abortions – conducted a surgical abortion under moderate sedation on Patient 3 without the use of ultrasound guidance. Staff A noted that the abortion was completed without difficulty and without complication, and also noted that the baby was 7 weeks gestation based on LMP (date of last menstrual period).
This violated Missouri law that requires the same physician do both the health assessment appointment and the abortion.
McNicholas, certified that she was present during Patent 3’s abortion, but when interviewed by DHSS investigators, McNicholas could not remember whether she was actually present.
Both the abortionist and the pathology lab indicated fetal parts were present during gross examination consistent with a baby that was 6 weeks and 6 days gestation, but McNicholas admitted she is not always present when the aborted baby remains are examined.
That means she really had no idea if the gross examination was done correctly by the trainee. The pathology lab admitted to competency issues regarding those conducting pathology reports during this time.
On August 24, a full month after her first abortion attempt, Patient 3 contacted RHS Planned Parenthood an told them she just returned from her doctor’s office and was told by her doctor that she was 12 weeks pregnant.
McNicholas conducted a second abortion on August 28, 2018, after a physical exam indicated the patient’s baby was 12-13 weeks gestation. No informed consent was obtained for the second abortion.
The Director of Surgical Services, Kawanna Shannon, was interviewed and admitted that, to her knowledge, they had never been contacted by the pathology lab regarding a failed or incomplete abortion.
Patient 12
Patient 12, was a 37-year old woman who was examined by an unknown RHS Planned Parenthood abortionist while at Washington University Hospital on April 16, 2019, where she had been admitted for vaginal bleeding at 21 weeks of pregnancy. She was diagnosed with placenta previa with possible placenta accreta and recommended for a late-term abortion. Patient 12 also had a history of a recent C-Section delivery, increasing her risk factors.
Placenta previa is a condition in which the placenta is located low in the uterus, covering all or part of the cervix. In many cases, this condition will resolve itself as the baby grows and the uterus expands, according to information noted in the Statement of Deficiencies.
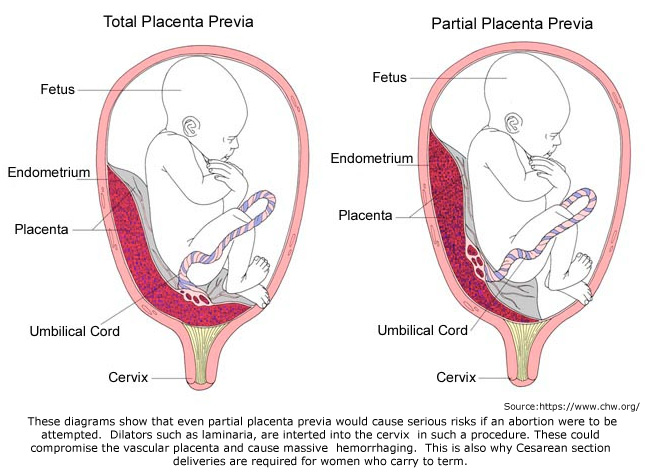
Placenta accreta, a condition where the placenta has grown too deeply into the uterine wall, added to Patient 12’s risk of hemorrhage during a second trimester abortion.
It is recommended that women with placenta previa deliver by Caesarean Section due to the heightened risks that include hemorrhaging because of the location of the placenta over the cervical opening.
However, contrary to accepted definitions of placenta previa, McNicholas describes it as a condition “in which the placenta was in the setting on a prior cesarean incision.”
This definition is incorrect and deceptive, but it does make it appear that committing an abortion on a woman with a high-risk 21-week pregnancy might actually be appropriate in an outpatient setting with no ability to cope with major hemorrhaging or other life-threatening complication that might arise.
According to the DHSS, ACOG standards state that a woman with Patient 12’s risk factors should have an abortion in a setting that has blood products readily available and has the capacity to conduct interventional radiology and/or hysterectomy. Even though RHS Planned Parenthood meets none one of those requirements, that is where Patient 12 was referred.
McNicholas brushed this aside, indicating that ACOG standards are merely suggestions meant to provide guidance, and do not reflect the standard of care.
A study done by the NIH noted that women who had placenta previa were more likely to experience heavy bleeding during second trimester abortions. This data contraindicates abortion for women in this condition, or at least provides a grim warning.

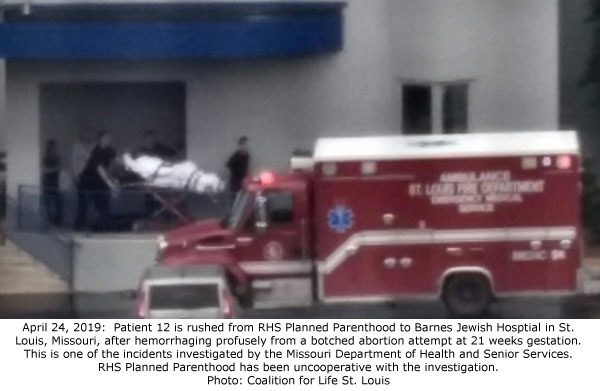
On April 24, 2019, laminaria insertion was attempted by Staff H, who noted the pregnancy was 20 weeks 4 days. During the process of inserting the dilators into the cervix at the start of what was expected to be a 2-day procedure, the patient experienced “brisk vaginal bleeding (EBL 200ml) requiring vaginal packing.” Blood loss of 200ml is roughly equivalent to nearly seven ounces.
The abortion attempt was halted and 911 was called for an emergency transport to her to Barnes Jewish Hospital. When she arrived at the hospital, according to the Statement of Deficiencies, the patient underwent an “emergency transfer to a hospital, where the patient was described as critically ill and suffering from shock, on pressors (drug for treating hypotension) and suffering massive blood loss.”
How massive? Patient 12 lost between 2 liters and 2.5 liters of blood – a life-threatening amount that represented over half her blood volume, which started at RHS Planned Parenthood.
McNicholas denied there was an emergency at RHS Planned Parenthood. She insisted that some bleeding occurred at the clinic, but it was a “small amount” and was under control and had stopped by the time the patient was transferred by ambulance.
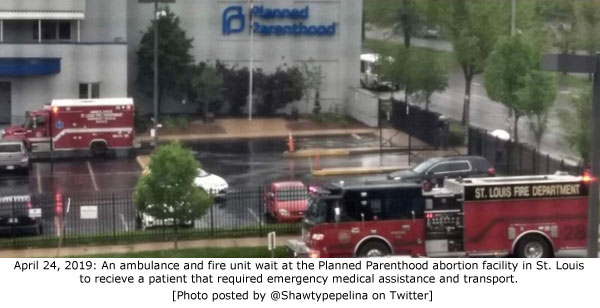
However, the vaginal packing likely just gave the appearance that the bleeding had stopped.
Operation Rescue has documented behavior like this before. For example, in the 2018 murder case of Robert Rho, a New York abortionist, there was testimony that Rho sutured the cervix and packed the vagina of a hemorrhaging abortion patient, then pretended like the bleeding had stopped. He released her and she bled to death a few hours later. Rho pleaded guilty to negligent homicide while the jury was in deliberations and was sentenced to 16 months to 4 years in state prison.
She instead shifted the blame onto Barnes Jewish Hospital where records indicated that Patient 12 underwent a uterine artery embolization, which is a surgical procedure wherein a blockage is injected into the uterine artery to control hemorrhaging. A Dilation and Evacuation abortion was conducted in the hospital’s OR. She was listed as “critically ill” and admitted to the Intensive Care Unit.
“One thing I’ve learned about abortionists who are in regulatory trouble is that they can be expected to spin the story to make them look like a hero, while everyone else is the villain. They are always the ones doing everything right, and they completely expect everyone to believe whatever cockamamie story they come up with because, as abortionists, they believe they are so politically protected that they can get away with it,” said Newman. “Here’s a word to the wise: Never believe a word that comes out of an abortionist’s mouth. In this case, the DHSS has all the files from Planned Parenthood and the pathology lab. They are well aware of what happened, although Planned Parenthood’s lack of cooperation may have left them wondering why. And that is what led to their decision that Planned Parenthood should not be licensed to do abortions.”
A hearing in this case has been extended to last five days and will now be held on October 28 – November 1, 2019, at the Wainwright State Office Building, 111 North 7th Street, Room 116, St. Louis, Missouri.






